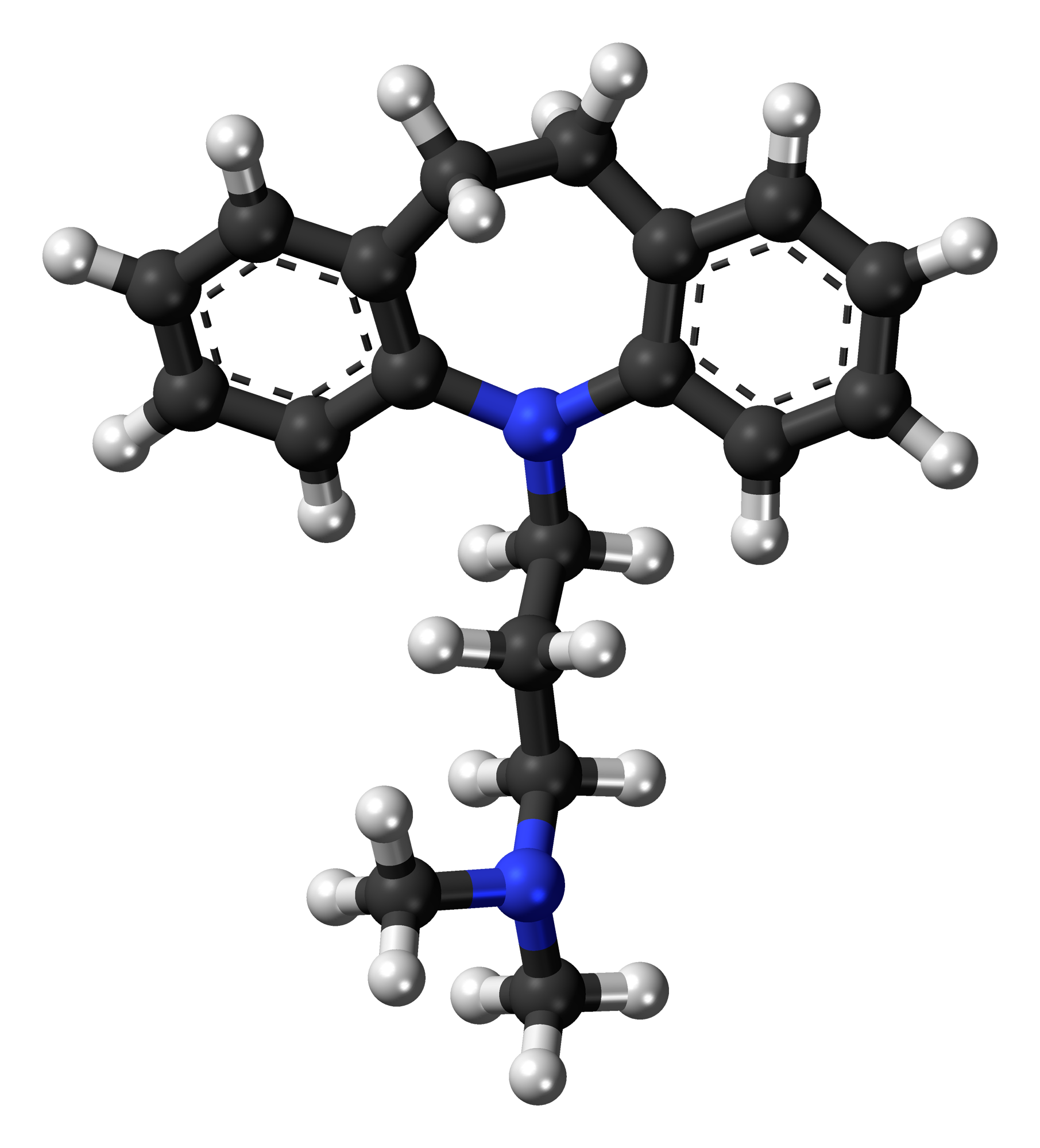
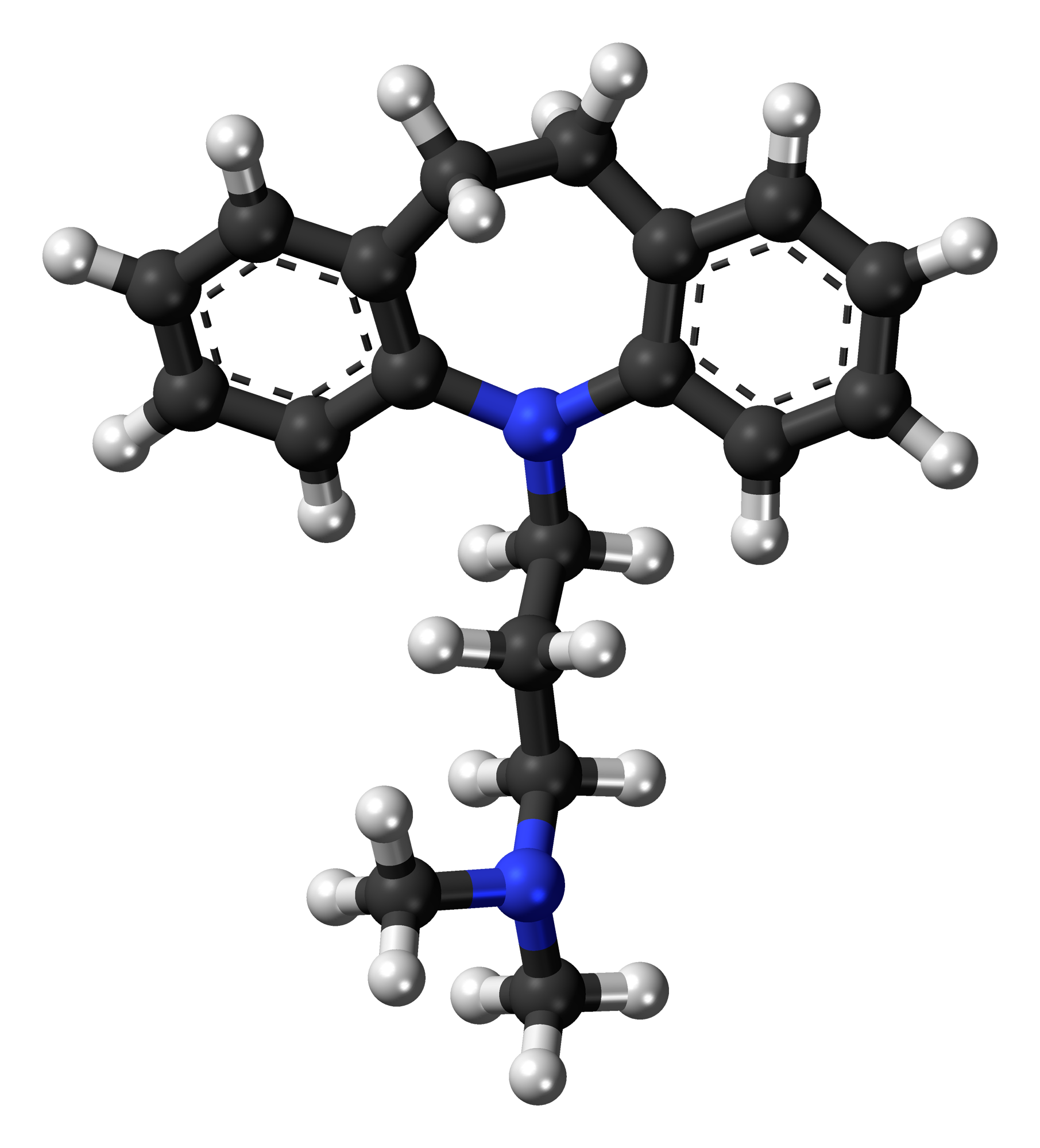
| name | Imipramine |
| Classification | Tricyclic antidepressant (TCA) |
| Pharmacokinetics | Imipramine is rapidly absorbed after oral administration. Peak plasma concentrations are usually reached within 2-8 hours. It is extensively metabolized in the liver, primarily by hydroxylation and N-demethylation. The major metabolites are also active. Imipramine is highly protein bound (approximately 95%). Elimination half-life is typically 12-36 hours, but can vary depending on individual metabolism and renal function. Imipramine and its metabolites are primarily excreted in the urine. |
| suggested dosage | | adult male 25 years 70kg | | initial | 25-50 mg daily, given in divided doses, with gradual titration upward as tolerated. | | maintenance | 50-150 mg daily, given in divided doses. Individual dosages will vary depending on patient response and tolerance. |
| | important notes | Dosage adjustments may be necessary based on patient response and side effect profile. Close monitoring by a healthcare professional is essential. |
|
| indications | Imipramine is used for the treatment of major depressive disorder (MDD), nocturnal enuresis (bed-wetting) in children, and other conditions. In cases of MDD, it may be useful for patients who do not respond well to other antidepressants. |
| safety in pregnancy | Imipramine use during pregnancy is generally not recommended due to potential risks to the fetus. The risks and benefits should be carefully considered by a healthcare professional if use during pregnancy is deemed essential. |
| safety in breastfeeding | Imipramine is excreted in breast milk. The potential risks to the infant should be weighed against the mother's clinical need for the medication. Consult with a healthcare professional for appropriate guidance. |
| side effects | | 1 | Dry mouth | | 2 | Constipation | | 3 | Blurred vision | | 4 | Urinary retention | | 5 | Orthostatic hypotension | | 6 | Drowsiness | | 7 | Sedation | | 8 | Weight gain | | 9 | Increased appetite | | 10 | Sexual dysfunction | | 11 | Tachycardia | | 12 | Cardiac arrhythmias | | 13 | Seizures | | 14 | Convulsions | | 15 | Tremor | | 16 | Confusion | | 17 | Hallucinations | | 18 | Jaundice | | 19 | Liver damage | | 20 | Leukopenia |
|
| alternatives | |
| contraindications | Known hypersensitivity to imipramine or other tricyclic antidepressants. Severe hepatic or cardiac disease. Patients with a history of seizures or recent myocardial infarction. Use with extreme caution in patients with glaucoma, prostatic hypertrophy, urinary retention, or severe respiratory impairment. |
| interactions | Imipramine can interact with a wide range of medications, including MAO inhibitors, anticholinergics, sympathomimetics, and certain other antidepressants. Specific interactions and their potential consequences should be reviewed by a healthcare professional. |
| warnings and precautions | Imipramine carries a risk of overdose, which can be life-threatening. Patients should be monitored closely for suicidal ideation or behaviors. Caution is advised in the elderly and patients with pre-existing cardiovascular conditions. Patients should be advised of the potential for orthostatic hypotension and appropriate measures taken to avoid falls. Careful monitoring of liver function and blood counts is crucial. |
| additional informations | Imipramine is a potent antidepressant but comes with a substantial side effect profile. A thorough discussion of potential risks and benefits is essential between the patient and prescribing physician. |
| patient specific considerations | | age | 25 years - No significant age-related adjustments in dosage are anticipated. | | weight | 70 kg - Dosage should be adjusted according to the patient's response and tolerability to the medication, as outlined in the suggested dosage section. | | gender | Male - Gender does not significantly alter the pharmacological properties or dosage of imipramine, but patient response and side effect profile will still vary. |
|