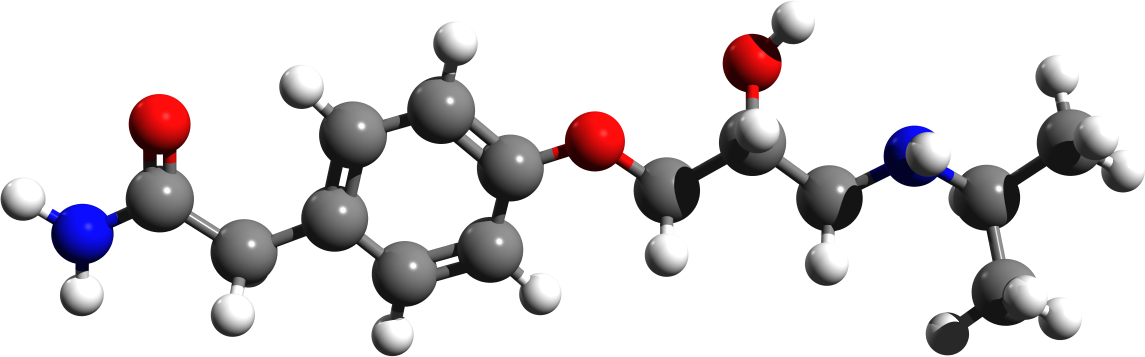
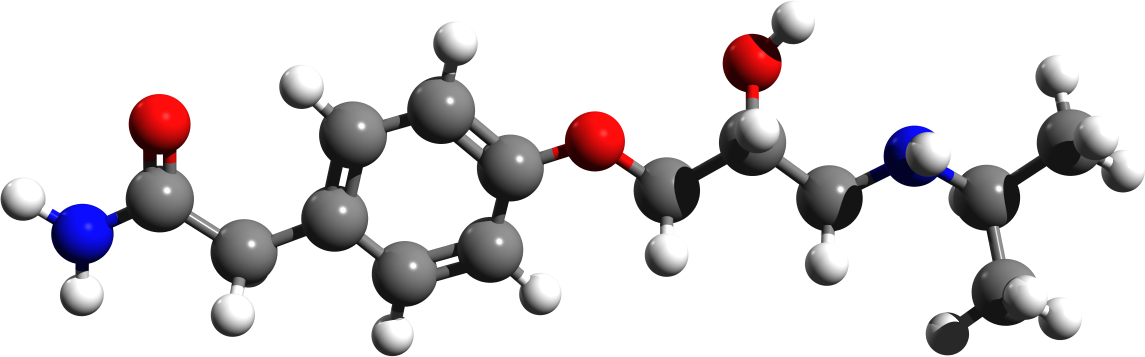
| name | Atenolol |
| Classification | Beta-blocker, Cardioselective |
| Pharmacokinetics | Atenolol is absorbed rapidly after oral administration. Peak plasma concentrations are generally reached within 2-4 hours. Atenolol is highly protein-bound (approximately 90%) in the blood and is extensively distributed in various tissues. The drug is metabolized primarily in the liver and is excreted mainly in the urine as metabolites. The elimination half-life is relatively long, ranging from 6 to 16 hours, allowing for once-daily dosing in many cases. These pharmacokinetic properties contribute to its efficacy in managing various cardiovascular conditions. However, individual variability in metabolism and clearance can affect drug levels. |
| suggested dosage | Initial dosage is typically 50 mg daily, which can be adjusted based on response. Maximum dosages can range from 100mg to 200mg per day, however, this should be guided by your healthcare provider. |
| indications | | 1 | Hypertension | | 2 | Angina pectoris | | 3 | Migraine prophylaxis | | 4 | Certain types of arrhythmias (e.g., supraventricular tachycardia) | | 5 | Post-myocardial infarction (to reduce risk of recurrent events) |
|
| Safety in pregnancy | Atenolol should be used during pregnancy only if the potential benefits outweigh the potential risks. It is not recommended for use during the first trimester or if there is a concern of a developing baby, and the potential risk to the baby. Consult with a healthcare provider. |
| Safety in breastfeeding | Atenolol passes into breast milk. The potential risks to the infant must be weighed against the benefits of treatment to the mother. It may be appropriate for use if the benefits outweigh the potential risks. Consult with a healthcare provider. |
| side effects | | 1 | Fatigue | | 2 | Dizziness | | 3 | Bradycardia (slow heart rate) | | 4 | Hypotension (low blood pressure) | | 5 | Cold extremities | | 6 | Bronchospasm (in patients with asthma or COPD) | | 7 | Constipation | | 8 | Sleep disturbances | | 9 | Sexual dysfunction | | 10 | Depression | | 11 | Dry mouth | | 12 | Nausea | | 13 | Vomiting |
|
| alternatives | |
| contraindications | | 1 | Severe bradycardia | | 2 | Cardiogenic shock | | 3 | Severe heart failure (in certain cases) | | 4 | Hypersensitivity to atenolol or other beta-blockers | | 5 | Sick Sinus Syndrome | | 6 | Severe Bronchospasm | | 7 | Second- or third-degree AV block (without a pacemaker) |
|
| interactions | | 1 | Other medications that can lower blood pressure or slow the heart rate (e.g., other antihypertensives, digoxin) | | 2 | Nonsteroidal anti-inflammatory drugs (NSAIDs) | | 3 | Verapamil | | 4 | Diltiazem |
|
| warnings and precautions | | 1 | Patients with asthma or chronic obstructive pulmonary disease (COPD) should be monitored carefully due to the risk of bronchospasm. | | 2 | Careful monitoring of blood pressure and heart rate is important, especially in the initial stages of treatment. | | 3 | Abrupt discontinuation of Atenolol may worsen angina or induce arrhythmias. Gradual dosage reduction is advised. Always discuss with your healthcare provider before stopping treatment. | | 4 | Patients with diabetes should be monitored closely, as atenolol may mask symptoms of hypoglycemia (low blood sugar). | | 5 | Patients with peripheral arterial disease or Raynaud's phenomenon should be monitored for potential exacerbation of symptoms. Patients with a history of severe chronic respiratory disease, such as COPD, should also be cautioned about potential exacerbations. |
|
| additional information | Atenolol is available in various forms (tablets, capsules). Dosage and duration of therapy should always be determined by your physician. Consult with your physician to discuss the appropriateness of Atenolol for your condition and to determine the most suitable dosage, duration, and any required monitoring. |
| patient details | |