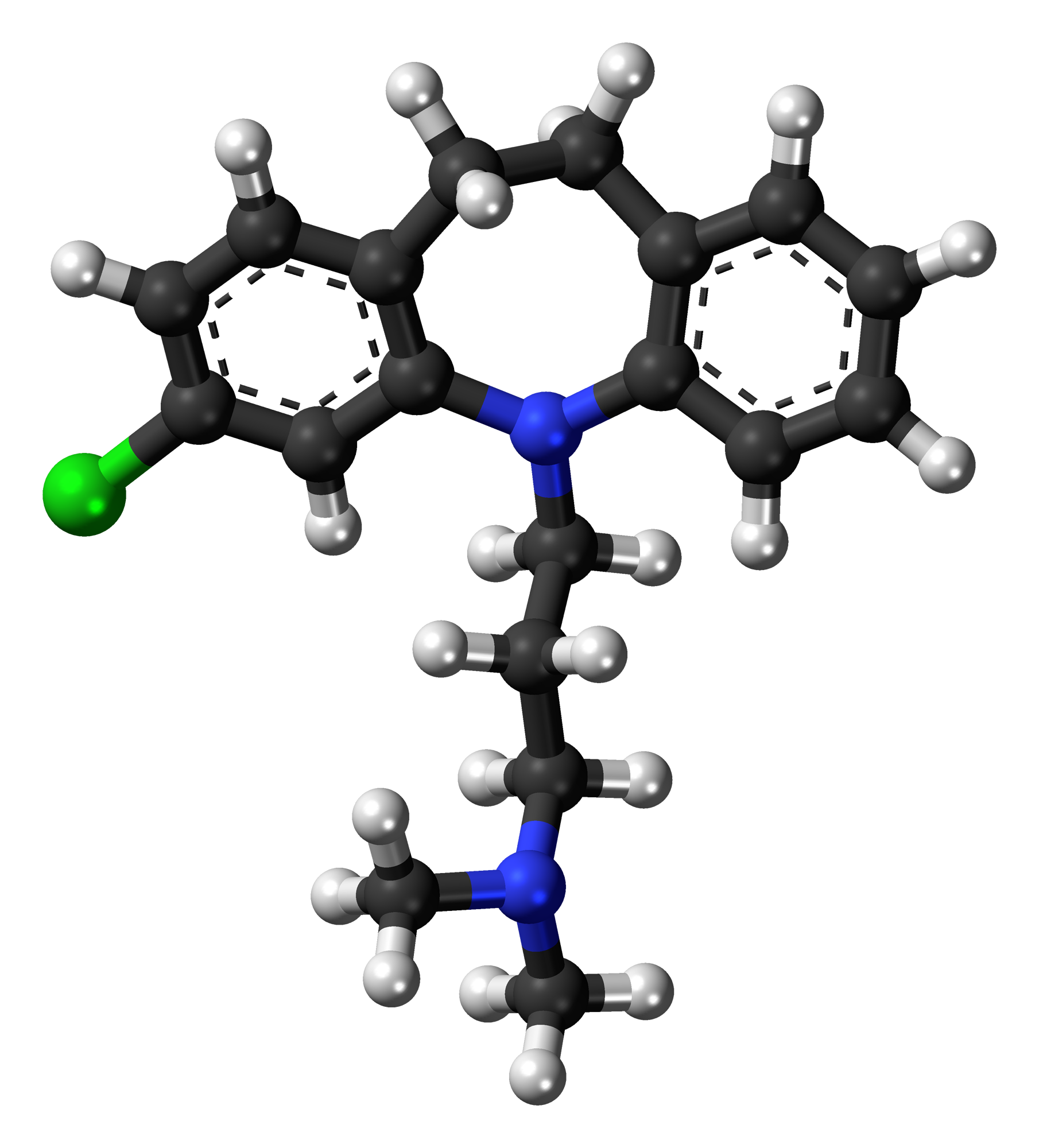
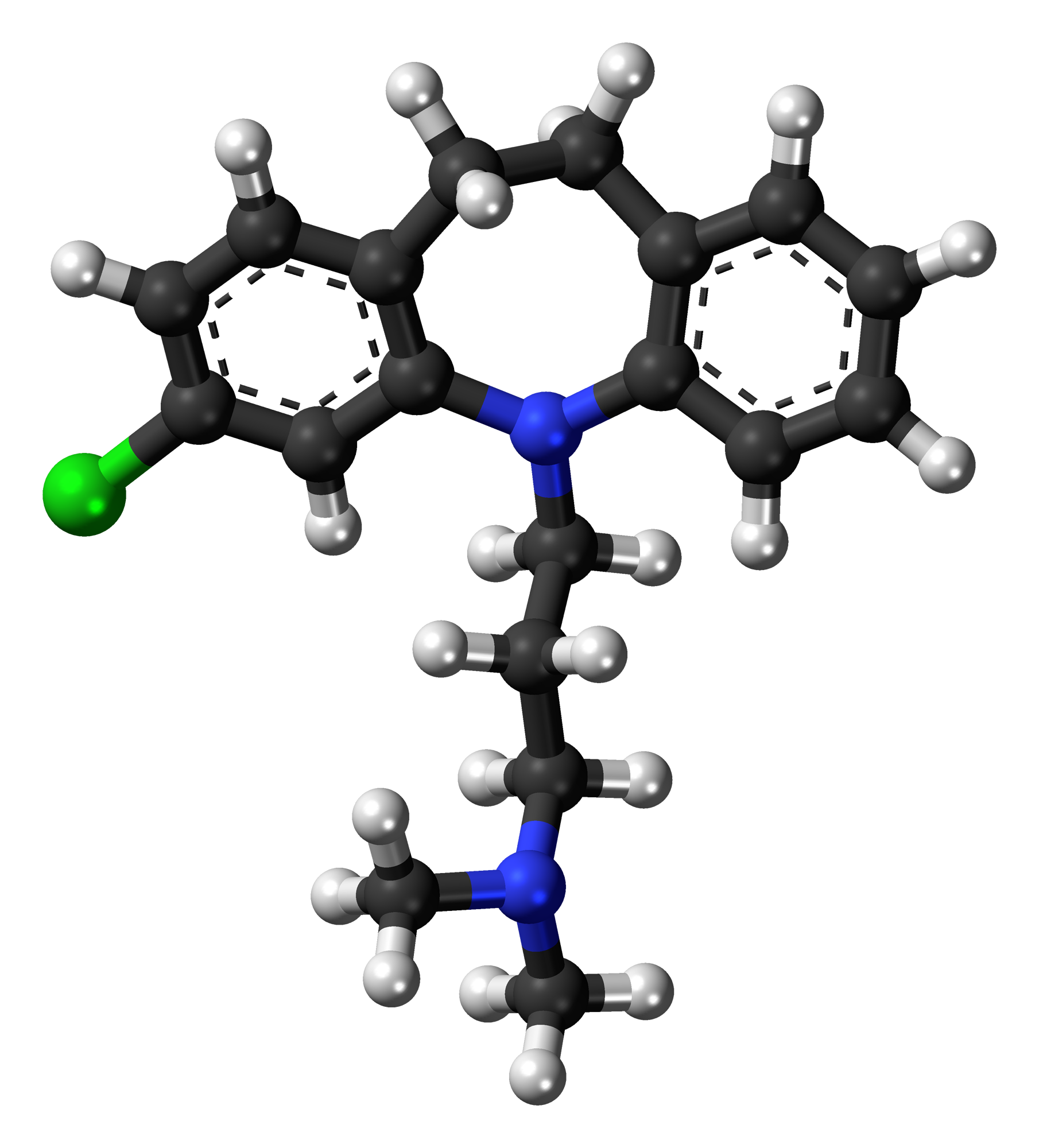
| name | Clomipramine |
| classification | Tricyclic Antidepressant (TCA) |
| pharmacokinetics | Clomipramine is a tricyclic antidepressant that is well absorbed orally. It undergoes significant first-pass metabolism in the liver. The primary metabolite, desmethylclomipramine, is also pharmacologically active. Distribution occurs throughout the body, and the drug is extensively bound to plasma proteins. Elimination occurs primarily through hepatic metabolism and excretion in urine. |
| suggested dosage | | male patient 25 70kg | | initial | 25-50mg/day, gradually increasing every 1-3 days, maximum 250mg/day | | note | Precise dosage depends on individual patient response and tolerance; start low and titrate slowly to avoid side effects |
| | general | | note | Dosage should be adjusted based on patient's response and tolerability to minimize adverse effects. | | consultation | Always consult with a qualified healthcare professional for personalized dosage recommendations. |
|
|
| indications | Clomipramine is primarily indicated for the treatment of obsessive-compulsive disorder (OCD). It may also be used in certain cases of depression, but newer, less side-effect prone antidepressants are usually preferred for that indication. |
| safety in pregnancy | Clomipramine use during pregnancy is associated with potential risks to the developing fetus. The benefits and risks should be carefully considered by the patient and their physician. It's important to monitor the pregnancy closely. The American Academy of Pediatrics and the American Psychiatric Association offer guidance on managing OCD in this population. **Consult your doctor immediately if you are pregnant or planning to become pregnant.** |
| safety in breastfeeding | Clomipramine may be excreted in breast milk. The benefits of breastfeeding versus the potential risks to the infant should be discussed with the physician. **Consult your doctor if you are breastfeeding or planning to breastfeed.** |
| side effects | | 1 | Anticholinergic effects (dry mouth, blurred vision, constipation, urinary retention) | | 2 | Sedation | | 3 | Weight gain | | 4 | Cardiac arrhythmias (especially in patients with pre-existing cardiac conditions) | | 5 | Seizures (especially at high doses) | | 6 | Hypotension | | 7 | Sexual dysfunction | | 8 | Drowsiness | | 9 | Tremor | | 10 | Tachycardia | | 11 | Mania/hypomania in susceptible patients |
|
| alternatives | |
| contraindications | | 1 | Known hypersensitivity to clomipramine or other TCAs | | 2 | Angle-closure glaucoma | | 3 | Severe cardiovascular disease (uncontrolled arrhythmias, conduction abnormalities, etc.) | | 4 | Severe liver disease | | 5 | Uncontrolled seizures | | 6 | Severe urinary obstruction |
|
| interactions | | 1 | Monoamine oxidase inhibitors (MAOIs): Potentially life-threatening interaction. Significant delay (at least 14 days) between stopping MAOI and starting clomipramine is necessary. | | 2 | Alcohol | | 3 | Other medications (especially those that affect the central nervous system or liver function) | | 4 | Avoid use with other serotonin-enhancing drugs due to possible serotonin syndrome |
|
| warnings and precautions | | 1 | Careful monitoring of patients with pre-existing cardiac conditions | | 2 | Close observation for suicidal ideation, particularly in the early phase of treatment | | 3 | Avoid abrupt discontinuation of the drug | | 4 | Use with caution in patients with a history of seizures or those taking medications that may lower seizure threshold. | | 5 | Monitor for signs of serotonin syndrome, especially when combined with other serotonergic drugs | | 6 | Monitor for signs of anticholinergic toxicity |
|
| additional informations | | 1 | Potential for overdose; keep out of reach of children. | | 2 | Patients should be instructed to report any unusual changes in mood or behavior | | 3 | TCAs have a narrow therapeutic index, and excessive doses may lead to serious side effects |
|
| patient specific considerations | | age | 25 years - generally safe, but requires careful monitoring. | | weight | 70 kg - suitable for typical dosing | | other health conditions | The presence of any other health conditions, such as cardiac conditions, or renal or liver disease, should be explicitly stated to and discussed with the prescribing physician. The patient's full medical history is crucial for appropriate use. |
|