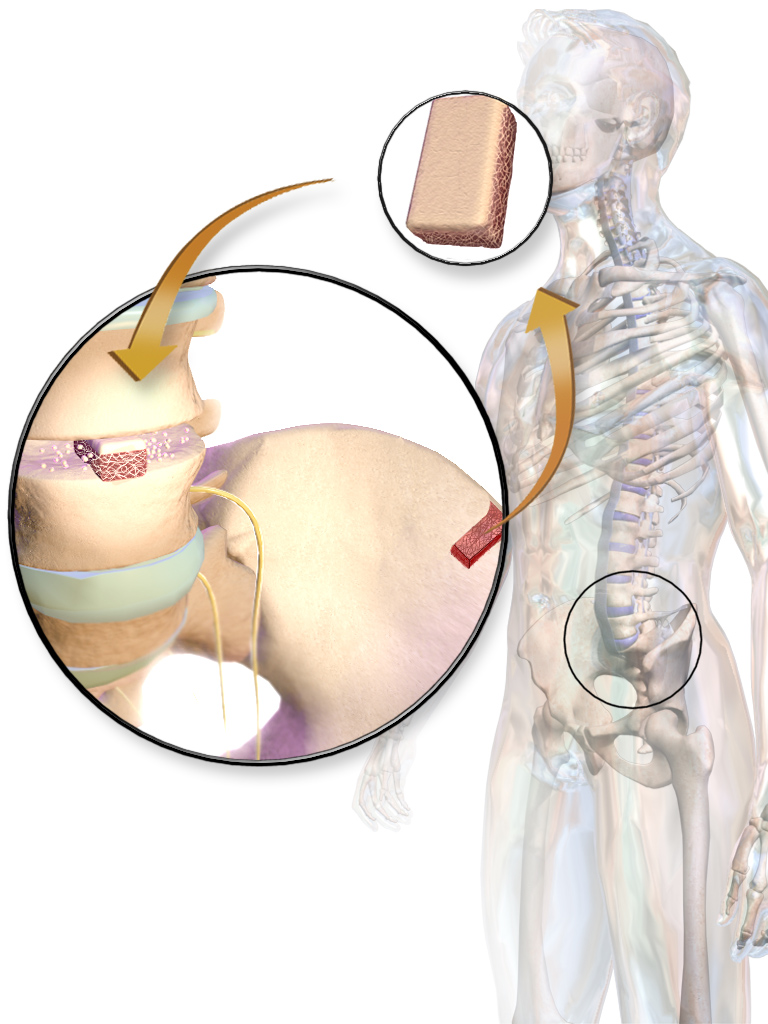
| drug name | Autograft Bone Grafts |
| classification | Surgical Technique/Biologic Material |
| pharmacokinetics | Not applicable. Autografts are not absorbed or metabolized in the body, but rather integrated into the surrounding tissue, though there is some resorption, remodeling, and remodeling of bone material. The time frame for this process depends on the site and type of graft. |
| suggested dosage | Not applicable. Dosage is determined by the surgeon based on the specific needs of the patient, including the size and location of the defect to be repaired. This is a highly individualized process and cannot be generalized. |
| indications | | 1 | Fracture repair | | 2 | Dental implant procedures | | 3 | Facial reconstruction | | 4 | Orthopedic procedures requiring bone replacement or augmentation | | 5 | Spinal fusion | | 6 | Bone defects (e.g., in craniofacial or maxillofacial procedures) | | 7 | Trauma with bone loss |
|
| safety in pregnancy | Limited data available. Autografts are not intrinsically harmful to a fetus; however, pregnancy is not a typical time to perform procedures necessitating autograft procedures. The potential risks and benefits should be carefully evaluated by both the patient and the surgeon, and the procedure should be performed only if clearly necessary. |
| safety in breastfeeding | Limited data available. There is no known direct harm to the nursing infant, but potential risks and benefits need to be assessed and the procedure performed only if necessary. |
| side effects | | 1 | Infection | | 2 | Bleeding | | 3 | Pain | | 4 | Swelling | | 5 | Delayed healing | | 6 | Non-union | | 7 | Graft resorption | | 8 | Implant loosening (in case of dental applications) | | 9 | Nerve damage (if grafts are near nerves) | | 10 | Possible hematoma formation |
|
| alternatives | | 1 | | alternative drug | Allograft Bone Grafts | | description | Utilizes bone from a donor source, often with processing to reduce risk of rejection, but there is potential for disease transmission and risk of immune response |
| | 2 | | alternative drug | Synthetic Bone Grafts | | description | Made from biocompatible materials. Effectiveness and integration vary depending on the specific material |
| | 3 | | alternative drug | Growth Factors | | description | Stimulate bone regeneration, often used in combination with other procedures or materials to improve outcomes |
| | 4 | | alternative drug | Platelet-Rich Plasma (PRP) | | description | Rich in growth factors which can stimulate bone healing, often used in conjunction with other procedures for enhanced effectiveness |
|
|
| contraindications | | 1 | Known hypersensitivity to bone graft material (if applicable) | | 2 | Active infection at the surgical site | | 3 | Severe bleeding disorders | | 4 | Uncontrolled medical conditions (e.g., diabetes, heart disease) | | 5 | Uncontrolled infection | | 6 | Poorly controlled systemic disease |
|
| interactions | Autografts do not interact with medications in a typical pharmacokinetic manner. However, other medications and procedures used in the same patient will influence outcomes. Consultation with the treating physician is essential. |
| warnings and precautions | | 1 | Potential for complications, such as infection, delayed healing, and non-union. | | 2 | Surgical procedure carries inherent risk | | 3 | Careful patient selection is essential, and the procedure should be performed only by qualified medical professionals. | | 4 | Precise surgical technique is important to optimize outcome. |
|
| additional informations | Autografts provide the greatest chance for successful long-term integration due to the patient's own body's cellular response; however, there are risks, and careful consideration of the patient and proposed surgical site should be undertaken by the physician. |
| patient data | |