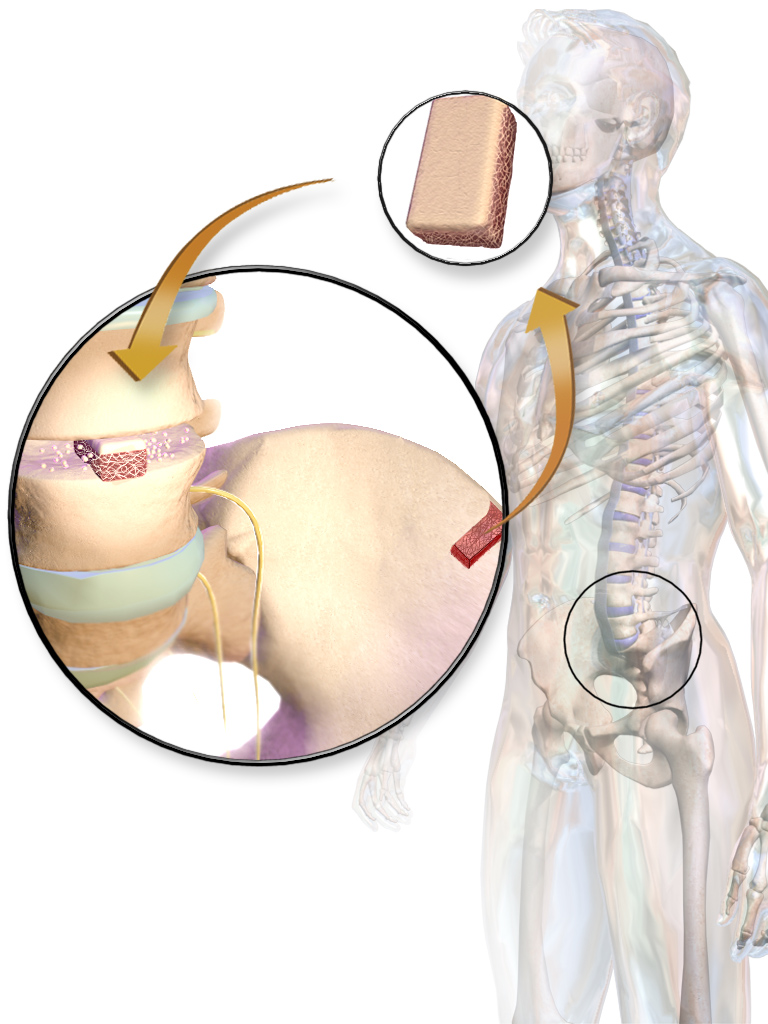
| drug | Allograft Bone |
| name | Allograft Bone |
| Classification | Biomaterial, Bone graft substitute |
| Pharmacokinetics | Allograft bone is not absorbed or metabolized in the body. It acts primarily as a scaffold for the body's own bone cells to regenerate new bone tissue. The body's natural healing processes determine the graft's resorption and integration over time. No specific pharmacokinetic data exists in the traditional sense. |
| suggestedDosage | Dosage and application are highly variable depending on the specific site and extent of bone defect/trauma. This information is best determined by a medical professional, considering the specific clinical presentation and needs of the patient. |
| indications | | 1 | Bone defects (e.g., fractures, nonunions, craniofacial defects) | | 2 | Orthopedic reconstruction | | 3 | Dental procedures (e.g., jaw reconstruction) | | 4 | Trauma repair | | 5 | Craniofacial abnormalities | | 6 | Bone regeneration in cases of critical-sized bone defects. |
|
| SafetyInPregnancy | Limited data, primarily from observational studies. The safety of allograft bone in pregnancy requires careful consideration by the treating physician. Potential risks to the fetus are not clearly established. Use in pregnancy should be based on a risk-benefit analysis and not routinely indicated. |
| SafetyInBreastFeeding | Limited human data. Allograft bone does not enter the maternal bloodstream significantly, and theoretically, there should not be a risk of passing to the infant through breast milk. However, further investigation is warranted to confirm this assertion. Use should be carefully considered, weighing risks and benefits for both mother and child. |
| sideEffects | | 1 | Infection (osteomyelitis): Risk exists if sterility/asepsis is not maintained. This may also be influenced by patient-specific issues and concomitant medications | | 2 | Pain at injection site | | 3 | Local swelling | | 4 | Recurrent or persistent pain | | 5 | Graft resorption | | 6 | Non-union (failure of bone healing) | | 7 | Graft rejection (less likely in allograft compared to autograft) | | 8 | Delayed healing (potential) | | 9 | Formation of scar tissue | | 10 | Fracture (potential if graft is not properly integrated) | | 11 | Inflammation | | 12 | Delayed bone maturation | | 13 | Formation of bone cysts | | 14 | Bone necrosis |
|
| alternatives | |
| contraindications | | 1 | Known hypersensitivity or allergy to the allograft material | | 2 | Active, untreated infection at the surgical site | | 3 | Uncontrolled medical conditions that could compromise healing | | 4 | Patient refusal |
|
| interactions | No known specific drug-drug interactions. However, concurrent treatments and underlying medical conditions may impact bone healing. Consult with a healthcare professional to discuss any potential interactions. |
| warningsAndPrecautions | | 1 | Proper surgical technique is crucial to avoid complications and maximize graft success. | | 2 | Patient history and current medical conditions should be carefully assessed. | | 3 | Post-operative monitoring and follow-up are essential to assess healing and to promptly manage any complications. | | 4 | Appropriate sterilization and handling procedures must be followed to minimize the risk of infection. |
|
| additionalInformation | Allograft bone products are usually derived from human donors and undergo various processing methods to reduce potential transmission risks. The choice between allograft and alternative bone grafts depends on a multitude of factors, including the specific patient's condition, the site of the defect, the availability of autografts, and the anticipated outcome. Careful evaluation and clinical judgment are paramount. |
| patientDetails | |