CT-Liver
Analysis Result generated by eMedify's MED AI
Click on "View Result" to view a detailed analysis generated by MED AI, with each analysis costing just between 5-20 INR (approximately 0.06 - 0.24 USD).

Analysis Result generated by eMedify's MED AI

• Report Type:
Abdominal CT Scan (likely contrast-enhanced), showcasing a lesion localized to the liver.
---
• Findings:
The provided CT scan image demonstrates a hypodense, well-circumscribed round lesion in the liver (likely in the right lobe). The lesion appears to have a fluid-filled or cystic appearance, as inferred from its homogeneous low-density characteristics. There are no evident signs of internal septations, calcifications, or irregular margins in the image provided. The surrounding hepatic parenchyma appears unremarkable, and there is no notable compression of adjacent structures.
---
• Differential Diagnoses with Probabilities:
1. Simple Hepatic Cyst: Probability: 70%
- Given the smooth, well-defined appearance of the lesion, a simple liver cyst is the most likely diagnosis. These are generally benign and asymptomatic unless they become large or infected.
2. Hydatid Cyst (due to Echinococcus granulosus infection): Probability: 20%
- There is a possibility of a parasitic origin, especially if the patient has exposure to endemic areas. Further testing with serology and imaging for daughter cysts or external calcifications is needed.
3. Liver Abscess: Probability: 5-10%
- The absence of rim enhancement or inflammatory changes around the lesion makes this less likely. However, in patients with fever or signs of infection, this diagnosis should be explored.
4. Hepatic Metastasis: Probability: <5%
- Metastatic lesions often present with irregular margins and heterogeneous characteristics, which appear absent in this case.
5. Polycystic Liver Disease: Probability: <5%
- Less likely unless multiple cysts are identified in association with kidney cysts or other systemic pathologies.
---
• Detailed Analysis:
The lesion's characteristics, particularly the smooth borders, homogeneity, and lack of enhancement (suggestive of non-solid content), are consistent with a benign hepatic cyst or parasitic involvement. The absence of septations or calcifications leans against complicated cysts or malignancies, such as metastasis. However, hydatid cysts can display similar imaging findings in early stages, necessitating serological confirmation or additional imaging for clarification.
---
• Recommendations:
1. Further Investigations:
- Serological tests: ELISA or indirect hemaglutination for Echinococcus antibodies.
- Follow-up imaging with contrast: Differentiation between simple cysts and other possibilities like infected cysts or abscesses.
- Liver function tests (LFTs): To assess any impact on liver function.
2. Symptom Tracking: Identify whether the lesion corresponds to any symptoms such as abdominal pain, fevers, or weight loss.
3. Aspiration or biopsy (Only if diagnosis remains unclear or symptoms persist): This should be performed under ultrasound or CT guidance and only if there's suspicion of abscess or malignancy.
---
• Treatment Options (if required):
1. Simple Hepatic Cyst: Observation, unless symptomatic. Large or symptomatic cysts may require laparoscopic cyst deroofing or aspiration.
2. Hydatid Cyst:
- Drugs: Albendazole or Mebendazole for parasitic control.
- Procedures: Percutaneous aspiration or PAIR (Puncture-Aspiration-Injection-Reaspiration) procedure under sterile conditions.
3. Liver Abscess: Empirical antibiotics like Ceftriaxone and metronidazole may be initiated pending cultures.
---
• Alarming Results:
- If serology for hydatid disease is positive, immediate treatment to prevent rupture and anaphylaxis is critical.
- Any evidence of rapid size increase, rupture, or compression of adjacent structures (e.g., bile duct obstruction) necessitates emergent intervention.
- Coexisting fever and inflammation could suggest abscess or infection, requiring immediate medical attention.
In conclusion, the lesion appears benign, with high likelihood of a hepatic cyst. However, ruling out parasitic infection through supportive testing is prudent. Further steps depend on clinical presentation and test results.

Analysis Result generated by eMedify's MED AI

• Report Type:
Chest X-Ray (Frontal view, labeled as "Right AP").
• Findings:
The image shows a large homogeneous opacity in the right lung field, likely in the upper lobe. The hilar region appears distorted, indicating potential pathology. No obvious pleural effusion is present on the right, and there are no apparent fractures or significant skeletal abnormalities in the ribs or vertebrae. The cardiac silhouette appears normal. Background lung fields demonstrate a potential reduction in aeration, with subtle streaking suggestive of interstitial involvement.
• Differentials and Probabilities:
1. Lung Cancer (Lung Cancer): 70% probability. Associated weight loss and poorly defined right upper opacity create a strong suspicion for malignancy.
2. Pulmonary Tuberculosis (Tuberculosis): 20% probability. Opacity with weight loss could indicate reactivation TB, given the apical involvement.
3. Infective Consolidation (Pneumonia): 10% probability. Although unlikely given the size and weight loss, a complex infective process cannot be excluded.
• Detailed Analysis:
The shadow in the right lung is worrisome for a malignancy due to its size, indistinct margins, and location in the upper lobe. The accompanying patient symptoms of weight loss are a significant red flag. The lack of other findings such as cavitation favors malignancy over tuberculosis. Additional diagnostic modalities are necessary to clarify the nature of this lesion.
• Recommendations:
1. CT Scan of the Chest: Required for detailed characterization of the lesion and to evaluate possible lymph node involvement or metastasis.
2. Bronchoscopy: For cytology/biopsy in case malignancy or granulomatous disease is suspected.
3. Sputum Analysis: Acid-fast bacillus (AFB) testing to rule out tuberculosis.
4. Blood Work: Complete blood count (CBC) and tumor markers like CEA for lung cancer investigation.
• Further Investigations:
- PET-CT: If malignancy is suspected, this will help stage the disease and identify metastasis.
- Biopsy: Either through bronchoscopy or CT-guided transthoracic needle aspiration.
• Alarming Results:
The combination of an upper lobe mass with systemic symptoms (weight loss) makes malignancy highly likely. Immediate evaluation and intervention are critical.
For more detailed information, consult references regarding lung cancer, tuberculosis, or pneumonia.

Analysis Result generated by eMedify's MED AI

• Report Type:
Dermatological Assessment
• Findings:
The image demonstrates a patch of erythematous (reddish), scaly, and slightly raised skin, indicative of an inflammatory process. There is evident peeling with a dry, flaky texture, which correlates with the patient's history of itching.
• Differentials with Probability Percentages:
1. Psoriasis (Plaque-type): ~70%
Features such as silvery-white scaling, erythema, and defined edges are highly suggestive of psoriasis.
2. Eczema (Atopic Dermatitis): ~20%
Similar appearance with itching, though lesions are often less defined and associated with a history of allergies or dry skin.
3. Fungal Skin Infection (e.g., Tinea Corporis): ~10%
Could mimic these findings but typically has a more well-defined edge and often displays central clearing.
• Detailed Analysis:
The appearance and symptoms most strongly align with plaque psoriasis due to its chronic nature, characteristic scaling, and itching. Psoriasis involves an autoimmune-related overproduction of skin cells, leading to accumulation and inflammation. It could be triggered by stress, infections, or environmental factors. However, fungal infection should be ruled out as some infections closely mimic psoriasis.
• Recommendations:
- First-line Treatment:
- Topical corticosteroids like Hydrocortisone or Betamethasone.
- Moisturizers and emollients to reduce dryness and scaling.
- Consider topical vitamin D analogs like Calcitriol.
- Lifestyle Adjustments: Avoid triggers such as stress, cold weather, and skin trauma.
- OTC Antihistamines to manage itching if severe.
• Further Investigations:
- Skin biopsy if diagnosis remains uncertain.
- Fungal culture and KOH testing to rule out a fungal infection.
- Blood tests (e.g., ESR, CRP) may help assess systemic inflammation if psoriasis suspicion is high.
• Alarming Results:
If the lesion enlarges rapidly, becomes infected (presence of pus, warmth, or fever), or unresponsive to initial treatment, escalate to a dermatologist. In the event of a potential significant systemic manifestation (e.g., psoriatic arthritis), early specialist intervention is warranted.
Analysis Result generated by eMedify's MED AI
• Report Type:
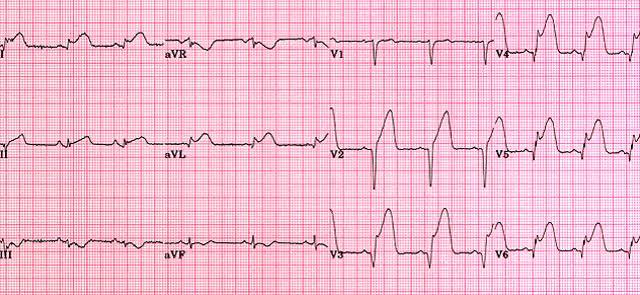
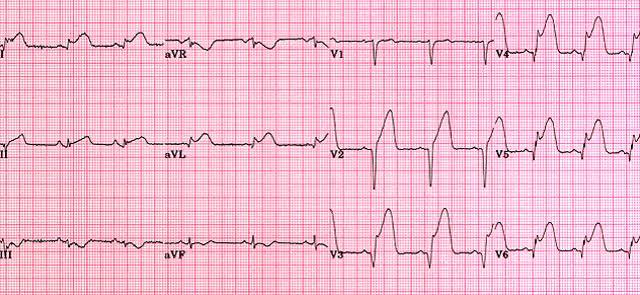
Electrocardiogram (ECG) Interpretation
• Findings:
This ECG demonstrates significant abnormalities that suggest acute myocardial ischemia or infarction. Specifically, there are:
1. ST-elevation in leads V1 to V6, as well as I and aVL, indicative of ST-Elevation Myocardial Infarction (STEMI), likely involving the anterior wall of the heart.
2. Reciprocal ST-segment depression is noted in the inferior leads (III and aVF), which further supports ischemia in a myocardial vascular territory.
3. The T waves are hyperacute in some leads.
4. There is no evidence of heart rhythm abnormalities like atrial fibrillation or ventricular tachycardia currently.
• Differentials with Probabilities:
1. Acute Anterior Wall STEMI (80%)
- Evidence: ST elevation in anterior leads (V1-V6), reciprocal changes, clinical correlation (pain).
- Related disease: Myocardial Infarction.
2. Pericarditis (10%)
- May show ST-elevation but typically has PR-segment depression and no reciprocal depression.
- Related disease: Pericarditis.
3. Severe Left Ventricular Hypertrophy (5%)
- May cause abnormal ST changes due to strain patterns, though typically without pain.
- Related disease: Left Ventricular Hypertrophy.
4. Hyperkalemia (5%)
- Can mimic these changes but would show peaked T waves and a characteristic widening QRS if severe.
• Detailed Analysis:
The distribution of ST-segment changes (anterior leads) aligns with myocardial ischemia in the territory supplied by the Left Anterior Descending (LAD) artery. Timely intervention is critical due to the likelihood of myocardial damage worsening without restoration of blood flow. This pattern is highly suggestive of emergent pathology such as STEMI.
Given the patient's history of pain (assumed to be chest pain) and these electrocardiographic findings, acute coronary syndrome is the most likely cause. This constitutes a medical emergency.
• Recommendations:
Immediate intervention and stabilization measures are critical:
1. Emergency Coronary Angiography and Revascularization:
- Preferably Percutaneous Coronary Intervention (PCI) to restore blood flow.
- Related procedure: Coronary Angioplasty.
2. Pharmacological Management:
- Start Aspirin and Clopidogrel to prevent clot propagation.
- Related drug: Aspirin, Clopidogrel.
- Administer Nitroglycerin for symptomatic relief, unless contraindicated.
- Related drug: Nitroglycerin.
- Heparin or related anticoagulants should be administered.
- Related drug: Heparin.
- Consider Beta-blockers unless the patient has contraindications like severe hypotension or bradycardia.
- Related drug: Metoprolol.
3. Laboratory Investigations:
- Cardiac biomarkers (troponin, CK-MB) to confirm myocardial damage.
- Complete blood work including electrolytes, lipid profile, and HbA1c to assess risk factors.
4. Echocardiography:
- Assess Left Ventricular Function and wall motion abnormalities.
5. Advanced Imaging:
- Post-stabilization, a CT coronary angiogram may help assess coronary artery anatomy.
• Alarming Results:
Immediate concern stems from:
1. The large territory of myocardial involvement indicated by extensive ST elevation.
2. The potential for cardiogenic shock or fatal arrhythmias like ventricular fibrillation if timely intervention is not performed.
• Treatment Options:
1. Primary PCI for reperfusion is the gold standard and should be performed urgently (within 90 minutes of first medical contact).
2. If PCI is unavailable, thrombolysis with fibrinolytics such as Tenecteplase or Alteplase may be considered.
- Related drug: Tenecteplase.
3. Post-reperfusion, long-term management involves:
- Statins (e.g., Atorvastatin) to control cholesterol.
- Related drug: Atorvastatin.
- Lifestyle modifications and cardiac rehabilitation.
• Conclusion:
This ECG strongly indicates an acute anterior wall STEMI, requiring emergent management to prevent irreversible myocardial damage. Immediate transfer to a cardiac care facility with PCI capability is recommended, alongside pharmacologic therapy to stabilize the patient en route.

Analysis Result generated by eMedify's MED AI

Below is the analysis based on the given patient history of back pain.
---
• Report Type:
MRI Lumbar Spine (T2-weighted sagittal view)
---
• Findings:
1. Disc Degeneration/Disc Desiccation:
Evidence of intervertebral disc degeneration is noted at the L4-L5 and L5-S1 discs. The reduced water content is indicated by the loss of hyperintense signals in these discs on the T2-weighted image.
2. Disc Herniation:
Mild posterior disc herniation is observed at the L4-L5 segment, causing indentation of the thecal sac. There is no significant canal stenosis or obvious nerve root compression.
3. Spinal Alignment:
The spinal alignment appears normal, with no evidence of scoliosis or kyphosis.
4. Facet Joint Arthropathy:
Mild degenerative changes are noted in the facet joints at the lower lumbar levels.
5. Spinal Cord and Neural Structures:
The spinal cord appears normal without any signs of myelopathy or intramedullary lesions. No significant foraminal narrowing is seen on this imaging plane.
6. Soft Tissue and Ligaments:
No abnormalities are noted in the surrounding ligaments, paraspinal muscles, or soft tissue structures.
---
• Differentials and Probability:
1. Degenerative Disc Disease - 80%
- Degenerative changes in the lumbar discs are consistent with this condition, which may correlate with the patient’s history of back pain.
2. Herniated Disc (Mild posterior herniation at L4-L5) - 50%
- While the herniation is mild, it could contribute to symptoms if nerve irritation occurs.
3. Lumbar Spondylosis - 40%
- Mild facet arthropathy may represent early spondylotic changes.
4. Sciatica - 20%
- Though not explicitly evident in these findings, radiating pain from compressive effects should be monitored and potentially correlated clinically.
---
• Detailed Analysis:
The findings in this MRI indicate chronic degenerative changes in the lower lumbar spine, particularly affecting the L4-L5 and L5-S1 levels. The loss of water content in the discs (desiccation) is typical for degenerative disc disease. Although the mild disc herniation at L4-L5 does not currently show signs of severe nerve impingement, it might contribute to back pain and potential radiculopathy, depending on further clinical correlation. The facet joint degeneration, while mild, may reflect early arthritic changes that could exacerbate pain with certain movements or postures.
---
• Recommendations:
1. Conservative Management:
- Physical therapy focusing on strengthening core muscles and improving flexibility.
- Use of analgesics or NSAIDs (e.g., ibuprofen) for pain relief.
2. Lifestyle Modifications:
- Weight management and ergonomic adjustments to reduce stress on the lumbar spine.
3. Further Investigations:
- If symptoms do not improve, a follow-up MRI with axial cuts and contrast could better evaluate any subtle nerve root involvement or inflammation.
- Electromyography (EMG) studies may be warranted if radiculopathy is suspected.
4. Interventional Options:
- If conservative measures fail, consider epidural steroid injections for persistent nerve-related symptoms.
- Surgical evaluation could be an option for severe, refractory cases with worsening neurological signs.
---
• Alarming Results:
While no immediate red flags such as fractures, severe spinal stenosis, or cauda equina syndrome are apparent, the patient should be monitored for any of the following symptoms:
- Progressive weakness or numbness in the lower limbs.
- Loss of bladder or bowel control.
- Severe, unrelenting pain unresponsive to conservative treatments.
If any of these symptoms develop, urgent imaging and neurosurgical consultation are recommended.
---

Analysis Result generated by eMedify's MED AI

This is an X-ray of the cervical spine in both Anteroposterior (AP) and Lateral views. Below is the detailed analysis of the report:
• Report Type:
X-ray of the Cervical Spine (AP and Lateral Views)
---
• Findings:
1. Alignment:
- The lateral view appears to show a loss of the normal cervical lordosis, which may indicate cervical spondylosis, muscular spasm, or an underlying injury.
- There may be slight anterior subluxation or malalignment of one or more cervical vertebrae, potentially suggesting a degenerative or traumatic etiology.
2. Disc Spaces:
- The intervertebral disc spaces in the cervical spine appear narrowed at certain levels, likely C4-C5 and C5-C6, which are common in cases of degenerative disc disease.
3. Bony Structures:
- Osteophytes (bone spurs) along the vertebral endplates, a hallmark of cervical spondylosis, are potentially visible.
- No evidence of acute fracture or dislocation noted from this resolution.
4. Soft Tissue:
- The prevertebral soft tissues appear unremarkable. No overt signs of mass effect or swelling suggestive of infection or malignancy.
5. Neural Foramina:
- Although specific neural foraminal narrowing is not clearly identified in plain X-ray, it is possible given the structural abnormalities noted. Clinical correlation for radiculopathy symptoms is advised.
---
• Differentials (with probability estimates):
1. Cervical Spondylosis (Degenerative Arthritis) - 70% Probability
- Age-related changes to vertebrae and discs, common in individuals >50 years.
- Link: Cervical Spondylosis
2. Cervical Disc Protrusion/Degeneration - 50% Probability
- Nerve compression complaints, if present, may be secondary to disc bulging or herniation.
- Link: Herniated Disc
3. Cervical Myelopathy (If Severe) - 30% Probability
- Central canal compression leading to spinal cord involvement.
- Link: Cervical Myelopathy
4. Trauma or Whiplash Injury (Muscle Spasm with Alignment Changes) - 20% Probability
- Could present similarly if a recent history of trauma exists.
---
• Detailed Analysis:
This X-ray reflects degenerative changes in the cervical spine typically associated with aging, particularly in females >50 years old. The narrowing of disc spaces and possible osteophytosis are suggestive of cervical spondylosis, which can cause neck pain, stiffness, and possible radiculopathy if nerve roots are compressed. The apparent loss of normal cervical curvature (straightening) also aligns with muscle spasm, often secondary to the degenerative process or injury.
While no acute findings (fracture/dislocation) are evident, clinical history of symptoms like radiating pain, limb weakness, or sensory deficits would further guide the assessment.
---
• Recommendations:
1. Further Investigations:
- MRI Cervical Spine: To evaluate soft tissue structures, including intervertebral discs and neural foramina, to assess nerve or spinal cord compression.
- Electromyography (EMG): If radiculopathy or nerve involvement is suspected, to localize the level of injury.
- Routine blood work (e.g., inflammatory markers) if inflammatory conditions like rheumatoid arthritis are suspected.
2. Treatment Options:
- Conservative Management:
- Physical therapy focusing on neck mobility and stability.
- Use of NSAIDs or analgesics, such as Ibuprofen or Diclofenac, for pain relief.
- Short-term muscle relaxants like Cyclobenzaprine for muscle spasm.
- Lifestyle Modifications:
- Ergonomic adjustments to workplace/posture.
- Strengthening exercises for the cervical spine.
- Interventional Procedures:
- If severe symptoms or MRI findings suggest nerve compression, consider steroid injections or surgical decompression (e.g., anterior cervical discectomy).
3. Alarm Signs to Address Immediately:
- Progressive neurological deficits (e.g., limb weakness, ataxia).
- Severe pain unrelieved by medications.
- Bowel or bladder incontinence, suggestive of severe spinal cord compression (Spinal Stenosis).
---
• Conclusion:
The findings on this cervical spine X-ray are most consistent with cervical spondylosis with secondary mechanical stress on soft tissues. While no immediate red flags are visible on the X-ray, further clinical history and advanced imaging are pivotal for a comprehensive assessment and management plan.

Analysis Result generated by eMedify's MED AI

Imaging Modality: X-ray and Ultrasound of Shoulder and Arm
Evidence of a comminuted fracture involving the proximal humerus with mild displacement noted.
Associated soft tissue swelling and joint effusion in the shoulder joint observed.
No evidence of dislocation or intra-articular loose bodies.
| Possible Condition | Probability (%) |
|---|---|
| Rotator Cuff Tear | 30% |
| Shoulder Fracture | 70% |
The comminuted fracture observed in the proximal humerus is consistent with the mechanism of injury described (fall injury). Associated soft tissue swelling indicates inflammatory response. While no signs of dislocation are evident, further clinical correlation with pain and range of motion is recommended.
If symptoms persist or worsen:

Analysis Result generated by eMedify's MED AI

• Image Analysis Report
•# Report Type: Lumbar Spine MRI (Magnetic Resonance Imaging)
•# Findings:
1. There appears to be disc desiccation and degeneration at the lumbar levels, particularly evident at L4-L5 and L5-S1. Disc bulging or herniation is noticeable, likely compressing adjacent neural structures such as the cauda equina or nerve roots.
2. Spinal canal narrowing (stenosis) is observed prominently at L4-L5, which corresponds to the patient’s complaints of tingling, numbness, back pain, and walking difficulty.
3. Foraminal stenosis, especially at L5-S1, suggests nerve root impingement, which explains the radicular symptoms in the legs.
4. No obvious fracture or malignancy noted; however, the structural abnormalities such as osteophytes or ligamentous hypertrophy could contribute to canal narrowing.
•# Differentials with Probability Percentages:
- Lumbar Disc Herniation: 70% - Strongly suggested by the visualized disc bulges and stenotic changes (Lumbar Disc Herniation).
- Lumbar Spinal Stenosis: 50% - The narrowing of the lumbar canal corroborates this diagnosis (Lumbar Spinal Stenosis).
- Sciatica: 40% - Compressive neural symptoms might cause sciatic nerve distribution pain (Sciatica).
- Cauda Equina Syndrome: 5% - Needs to be ruled out urgently if there’s bowel/bladder dysfunction (Cauda Equina Syndrome).
•# Detailed Analysis:
The degeneration and disc pathology found in this MRI correlate with the described symptoms. The nerve impingement at L4-L5 or L5-S1 is likely impeding motor and sensory nerve functions, causing walking difficulties and numbness. The back pain and radicular symptoms appear to be stemming from mechanical compression rather than inflammatory processes.
•# Recommendations:
- Start with conservative treatment options like physical therapy, NSAIDs (e.g., Ibuprofen), and possibly Gabapentin or Pregabalin for neuropathic pain (Gabapentin, Pregabalin).
- If no improvement is seen in the next 4-6 weeks, consider epidural steroid injections.
- Surgical options (e.g., lumbar decompression or discectomy) may be explored in severe cases or if progressive neurological deficits develop.
•# Further Investigations:
- Conduct nerve conduction studies (NCS) to evaluate the extent of nerve damage.
- Consider a follow-up MRI with contrast for detailed imaging of nerve roots if symptoms worsen.
- Rule out metabolic or systemic conditions contributing to neuropathy.
•# Alarming Results:
- Progressive weakness or impaired bowel/bladder function should raise suspicion for Cauda Equina Syndrome, which is a surgical emergency and requires immediate attention.
By promptly addressing these findings, symptom relief and prevention of progression can be achieved. Please consult an orthopedic spine specialist or a neurologist for further guidance.

Analysis Result generated by eMedify's MED AI

Medical Image Analysis Report
Report Type: Radiograph of the Left Wrist (AP and Lateral View).
Findings:
The X-ray depicts a fracture of the distal radius with associated disruption of the cortical continuity. The alignment shows a comminuted fracture, with probable dorsal angulation as suggested in the lateral view. Additionally, there is involvement of the radiocarpal joint space, indicating the possibility of intra-articular extension of the fracture.
There is also an apparent shortening and possible displacement of the distal radial fragment. The ulnar styloid process appears unremarkable; however, it warrants careful evaluation in a clinical setting. No evident foreign body or associated soft tissue calcification is noted within the reach of this radiographic field.
Differential Diagnoses:
1. Distal Radius Fracture (Colles’ Fracture): (95% probability) - This is the most probable diagnosis given the cortical disruption, comminution, and dorsal angulation.
Colles' Fracture
2. Smith’s Fracture: (5% probability) - Usually involves volar angulation; the existing dorsal angulation makes this less likely.
Smith's Fracture
Detailed Analysis:
This image is highly indicative of acute post-traumatic fracture secondary to the patient’s history of a fall. Among distal radius fractures, Colles’ fracture is predominant in this scenario, characterized by dorsal angulation and a displaced and comminuted fracture. Intra-articular extension increases the complexity of such fractures and may lead to long-term complications, such as post-traumatic arthritis.
The fracture pattern suggests significant force transmission during the fall, likely involving an outstretched hand. Alignment abnormalities require immediate correction to restore proper wrist function.
Recommendations:
1. Immediate Orthopedic Evaluation: For clinical correlation and assessment of neurovascular compromise, particularly focusing on the median nerve, given possible swelling or compression.
2. Closed or Open Reduction Consultation: Depending on the degree of displacement.
3. Further Investigations: Consider a CT scan of the wrist for detailed evaluation of intra-articular extension and pre-surgical planning.
4. Splinting and Immobilization: Initially recommended with a well-molded plaster cast to prevent further displacement and to allow for swelling control.
Treatment Options:
- Non-operative Management: For minimally displaced fractures without major articular involvement, conservative treatment involving immobilization with a cast is sufficient. This may include pain control with medications such as ibuprofen.
- Surgical Intervention: If displacement is severe or articular involvement is prominent, open reduction and internal fixation (ORIF) with plates or pins may be required.
Alarming Results:
1. Intra-articular involvement and alignment irregularities raise the risk of long-term functional impairment (e.g., reduced range of motion, grip strength).
2. The possibility of compartment syndrome, though rare in wrist fractures, warrants monitoring for signs like persistent swelling and pain.
Further Recommendations:
Physical therapy should be initiated post-immobilization or post-surgery to prevent stiffness and ensure a functional recovery. Continuous follow-up with repeated imaging to monitor fracture healing is also essential.
UK: +44 121 823 1220
USA: +1 628-300-0016
IN: +91 78375 59525
® 2025 Med MD. All rights reserved